The SCAI Consensus Statement on the Management of Calcified Coronary Lesions aimed to create an algorithmic approach to treating calcified CAD. The purpose of the publication was to put forth an expert consensus document regarding methods to identify types of calcified coronary lesions, a central algorithm to help guide use of the various calcium modification strategies, tips for when using each treatment modality, and a look at future studies and trials for treating this challenging lesion subset. In this Q&A, we invited Dr. Deepthi Sudhakar, Sharp Memorial Hospital, San Diego, CA and the Committee Co-Chair of SCAI WIN, to share her insights on the algorithm’s recommendations and its impact on her daily practice.
Download the SCAI Algorithm
What was your algorithm before you came across the SCAI Algorithm1?
Dr. Sudhakar: The SCAI expert consensus statement on the management of calcified coronary lesions provides valuable guidance on the management of severely calcified lesions, which are amongst the most challenging cases we encounter. With all the tools now available for plaque modification and variability in lesion types, this document distills the management of a complex subset of lesions into a streamlined algorithm. I frequently use intravascular imaging for guiding lesion preparation; however, since reviewing this algorithm, I have increased my use of imaging after modification to assess adequacy. I have also increased the use of more than one tool for lesion preparation.
How important is it to have society guidance on things like calcium specifically?
Dr. Sudhakar: We are seeing increasingly higher rates of complex calcified lesions and restenosis lesions, and this, coupled with the advancement of new technologies for plaque modification, has led to a lot of heterogeneity in our understanding and management of these lesions. The publication of this statement is well-timed and serves a need for a thoughtful, standardized approach to these lesions. Importantly, it highlights that not all calcified lesions are created equal, and modification is not a one-size-fits-all approach. There is a lot of emphasis placed on imaging to understand the subset of calcified lesions before deciding on a modification strategy. This is key to choosing the most appropriate modification strategy for better long-term outcomes. It is comprehensive and encompasses several types of lesions, such as bifurcation lesions and chronic total occlusions.
Is there anything you’d change or add to the current algorithm?
Dr. Sudhakar: Expand on the subsets of lesions where you might want to combine different modalities for calcium modification. The scarcity of existing data limits some of this, so it will be very interesting to see how the results of ongoing trials like ECLIPSE (NCT03108456), ROLLING-STONE (NCT05016726), SHORT-CUT (NCT06089135), and ROLLERCOASTR (NCT04181268) add to our understanding of modification. The addition of restenosis lesions to the algorithm would also be helpful. While more tools are available for calcium modification, not all are widely available. I think that is an important aspect to keep in mind when adopting any algorithm. The setting where lesion preparation occurs and hemodynamics are also important factors to remember.
How important is imaging in your algorithmic approach to calcium?
Dr. Sudhakar: Imaging is crucial in any percutaneous coronary intervention, especially with calcified lesions. As the document clearly states, multiple calcified lesions and outcomes vary despite adequate preparation in some cases, such as eruptive nodules. We must understand what we are treating specifically before choosing the right modality. This is particularly true in restenosis lesions, where understanding the mechanism is critical to lesion preparation.
Was there anything about your approach or a device that the SCAI Algorithm changed?
Dr. Sudhakar: I frequently use intravascular imaging; however, this document led me to focus on more aspects of a lesion outside of arc length, such as the type of calcified nodule and depth of calcium. I have also increased my use of imaging after lesion preparation to ensure fracture and check for dissections in eccentric lesions. In contrast, before the document, I relied more often on expansion with non-compliant balloons after modification to determine the adequacy of preparation. I have also increased my use of combining atherectomy with intravascular lithotripsy in treating these lesions.
Are there any challenges you encounter with calcium that may not have a current treatment paradigm?
Dr. Sudhakar: Bifurcation lesions with severe calcification and restenosis lesions with protrusion of calcified nodules remain challenging subsets to treat.
Do you follow a mental step-by-step process, and if so, when does that kick in? After imaging or upon visualization by angio?
Dr. Sudhakar: A patient’s age and underlying comorbidities are factors I consider even before the initial angiogram in forming my pre-test probability of calcified disease. On the initial angiogram, I am focusing on calcification, tortuosity at the lesion, the presence of bifurcation lesions, and estimates of vessel size. Calcification on angiography, particularly if there are eccentric lesions, shows me that I need to assess for calcified nodules when imaging. I rely on intravascular imaging to guide my modification strategy. Still, my decision also heavily depends on the patient’s characteristics, hemodynamics, and ability to tolerate one modification tool versus another.
What data do you think are still needed to verify or support the algorithm?
Dr. Sudhakar: We have some data to support the use of atherectomy with intravascular lithotripsy; however, there needs to be long-term data, which the ongoing trials should shed some light on. Sex differences in how we treat calcified lesions are another area where we lack data, which calls for increasing enrollment in clinical trials. In this regard, EMPOWER (NCT05755711) may be able to shed some light on this topic.
[1] Riley, Robert F., Mitul P. Patel, J. Dawn Abbott, Sripal Bangalore, Emanouil S. Brilakis, Kevin J. Croce, Darshan Doshi, et al. “SCAI Expert Consensus Statement on the Management of Calcified Coronary Lesions.” Journal of the Society for Cardiovascular Angiography & Interventions 3, no. 2 (February 2024): 101259. https://doi.org/10.1016/j.jscai.2023.101259
Dr. Deepthi Sudhakar is a paid consultant of Shockwave Medical.
Views expressed are those of the physician and not necessarily of Shockwave Medical. Dr. Deepthi Sudhakar is a paid consultant for Shockwave Medical. See important safety information below.
Coronary Important Safety Information:
Please contact your local Shockwave representative for specific country availability and refer to the Shockwave C2 and Shockwave C2+ instructions for use containing important safety information.
In the United States: Rx only
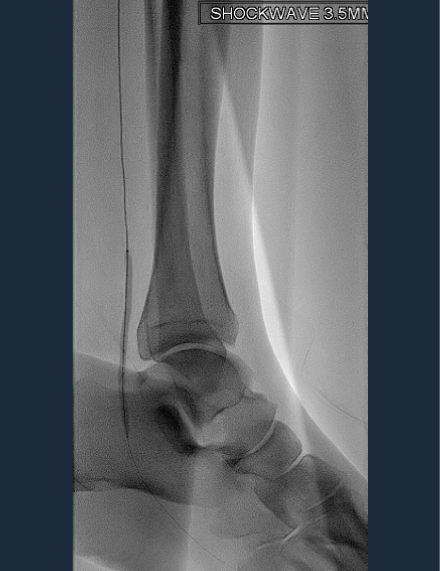
Indications for Use—The Shockwave Intravascular Lithotripsy (IVL) System with the Shockwave C2 Coronary IVL Catheter is indicated for lithotripsy enabled, low-pressure balloon dilatation of severely calcified, stenotic de novo coronary arteries prior to stenting.
Contraindications—The Shockwave C2 Coronary IVL System is contraindicated for the following: This device is not intended for stent delivery. This device is not intended for use in carotid or cerebrovascular arteries.
Warnings— Use the IVL Generator in accordance with recommended settings as stated in the Operator’s Manual. The risk of a dissection or perforation is increased in severely calcified lesions undergoing percutaneous treatment, including IVL. Appropriate provisional interventions should be readily available. Balloon loss of pressure was associated with a numerical increase in dissection which was not statistically significant and was not associated with MACE. Analysis indicates calcium length is a predictor of dissection and balloon loss of pressure. IVL generates mechanical pulses which may cause atrial or ventricular capture in bradycardic patients. In patients with implantable pacemakers and defibrillators, the asynchronous capture may interact with the sensing capabilities. Monitoring of the electrocardiographic rhythm and continuous arterial pressure during IVL treatment is required. In the event of clinically significant hemodynamic effects, temporarily cease delivery of IVL therapy.
Precautions— Only to be used by physicians trained in angiography and intravascular coronary procedures. Use only the recommended balloon inflation medium. Hydrophilic coating to be wet only with normal saline or water and care must be taken with sharp objects to avoid damage to the hydrophilic coating. Appropriate anticoagulant therapy should be administered by the physician. Precaution should be taken when treating patients with previous stenting within 5mm of target lesion.
Potential adverse effects consistent with standard based cardiac interventions include– Abrupt vessel closure – Allergic reaction to contrast medium, anticoagulant and/or antithrombotic therapy-Aneurysm-Arrhythmia-Arteriovenous fistula-Bleeding complications-Cardiac tamponade or pericardial effusion-Cardiopulmonary arrest-Cerebrovascular accident (CVA)-Coronary artery/vessel occlusion, perforation, rupture or dissection-Coronary artery spasm-Death-Emboli (air, tissue, thrombus or atherosclerotic emboli)-Emergency or non-emergency coronary artery bypass surgery-Emergency or non-emergency percutaneous coronary intervention-Entry site complications-Fracture of the guide wire or failure/malfunction of any component of the device that may or may not lead to device embolism, dissection, serious injury or surgical intervention-Hematoma at the vascular access site(s)-Hemorrhage-Hypertension/Hypotension-Infection/sepsis/fever-Myocardial Infarction-Myocardial Ischemia or unstable angina-Pain-Peripheral Ischemia-Pseudoaneurysm-Renal failure/insufficiency-Restenosis of the treated coronary artery leading to revascularization-Shock/pulmonary edema-Slow flow, no reflow, or abrupt closure of coronary artery-Stroke-Thrombus-Vessel closure, abrupt-Vessel injury requiring surgical repair-Vessel dissection, perforation, rupture, or spasm.
Risks identified as related to the device and its use: Allergic/immunologic reaction to the catheter material(s) or coating-Device malfunction, failure, or balloon loss of pressure leading to device embolism, dissection, serious injury or surgical intervention-Atrial or ventricular extrasystole-Atrial or ventricular capture.
Prior to use, please reference the Instructions for Use for more information on warnings, precautions and adverse events. https://shockwavemedical.com/IFU