Q&A with Dr. Dean Kereiakes about the DISRUPT CAD III 1yr Data at TCT21
Following its presentation at TCT21 in a featured clinical research session, we caught up with DISRUPT CAD III co-principal investigator, Dean Kereiakes, M.D., FACC, FSCAI, Medical Director of The Christ Hospital Heart and Vascular Center and the Christ Hospital Research Institute; Professor of Clinical Medicine, The Ohio State University, to get his thoughts on the data and what stands out from his perspective since the primary 30-day outcomes were presented at TCT20.
What is the significance of the one-year follow-up data from the DISRUPT CAD III study, which was included by TCT as one of the meeting’s best abstracts in the featured clinical research session?
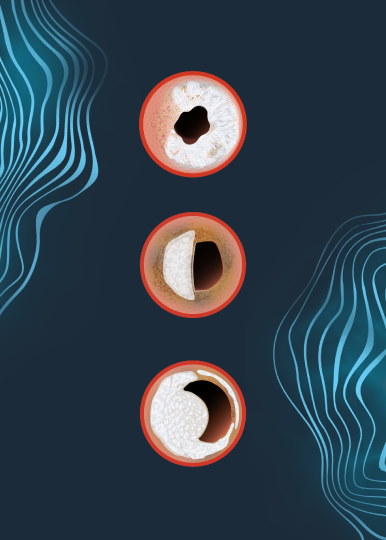
Dr. Kereiakes: I think it’s very significant that it shows sustained and persistent relative benefit of IVL for lesion preparation prior to coronary stenting. Since this is the first robust one-year data that has been presented on coronary IVL, I think that’s very important as there were concerns, as there have been with the use of ablative technologies, that in late follow-up there might be some loss of the benefit that might have been predicted by the MSA and percent stent expansion at the initial procedure. These were phenomenal levels from the OCT sub study – 102% stent expansion and MSA of 6.5mm2 at the site of maximum lesion calcification. The fact that we were able to achieve these excellent levels, one would predict based on all other previous imaging studies, that there should be a low rate of TLR and stent thrombosis, which is exactly what we found.
Were there any other concerns that you had about the potential one-year outcomes going into TCT?
Dr. Kereiakes: Well, some had expressed concerns that there might be a negative impact of the energy generated by IVL like we see with the friction induced by rotational and orbital atherectomy. The reassuring answer is it doesn’t look like it as the data are great. When, at 1-year, you have an ID-TLR of 4.3% and a total stent thrombosis rate of 1.1% with only one patient (0.3%) having a stent thrombosis beyond 30 days, that bodes very well.
Was there anything surprising to you about the data itself?
Dr. Kereiakes: No, I actually thought it was predictable based on the optimized stent implantation results we were able to achieve by pretreating these severely calcified lesions – 100% of which were classified as severely calcified as adjudicated by an independent core lab.
Now that durable one-year outcomes have been shown, where do we go from here from a clinical research perspective?
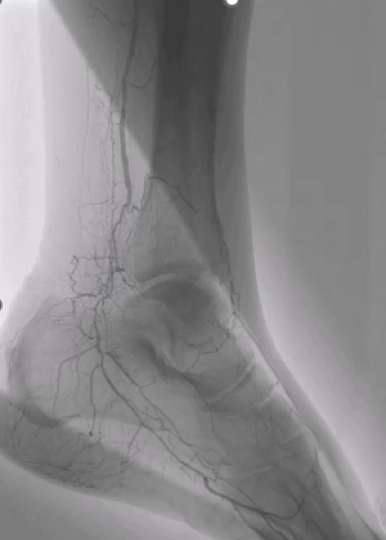
Dr. Kereiakes: I think the next step is to analyze the post-market approval study being done through the ACC CathPCI registry, which is very innovative. I think this is going to be very helpful to expand the observations using IVL for lesion preparation in a much broader population of real-world patients.
Given that this was a single arm study, how do you contextualize the results of the one-year findings?
Dr. Kereiakes: You know I think without a randomized comparator it’s always challenging and difficult. Recall that we set up the best performance goals you could possibly set up using a similar population, similar definitions and similar endpoints, to be identical to ORBIT II which was the pivotal trial for FDA approval of orbital atherectomy. This was probably the best designed non-randomized comparator possible. That said, although it remains a cross trial, non-randomized comparison, when you look at the one year data, you’ve got Disrupt CAD III at 13.8% MACE rate and 16.9% for ORBIT II. This is a very intriguing, hypothesis-generating but non-randomized comparison.
For those physicians that may have been waiting for longer term data to prove out the effectiveness of the therapy, what would you tell them now that the one-year data is available?
Dr. Kereiakes: I’d tell them to look at the data and look at the best data from the other sources of calcium modifying technologies – take in the totality of the data. That means peri-procedural results to 30-days and at one year. There’s never been a cohort of patients with more severely calcified target lesions than those enrolled in DISRUPT CAD III for U.S. FDA approval of coronary IVL. When you look at the substrate that was enrolled and you look at the peri-procedural outcomes, with zero perforations, zero abrupt closures, zero no re-flow with IVL alone and only one patient with an Ellis type 1 micro-perforation following stent deployment which sealed by itself out of the entire series. When I look at these data I say you have a low complication rate, great outcomes at 30 days that now persist out to one year. Knowing these data, going forward I would hesitate to approach severely calcified target lesions without IVL.
Is there anything else that stood out to you about the IVL data presented at TCT?
Dr. Kereiakes The other thing that I would honestly say, that’s really hard to recreate, is that when you look at all of the IVL data, we have 47 sites in four countries with DISRUPT CAD III and an additional pooled analysis of data from 72 sites in 12 countries. When you look at all of these different sites across multiple continents and countries, there is remarkable consistency in the safety and effectiveness endpoints achieved. I think that reflects the ease-of-use of IVL. It’s a balloon. Every interventionalist, I don’t care what subspecialty you are, uses balloons. And that’s the relative safety of the technology as well. Delivering high technology in a primitive delivery system. It doesn’t matter whether you’re in Europe or U.S. Doesn’t matter if you’re in a big center, or little center. The beauty of this observation is the consistency of safety and effectiveness. We found no differences with IVL. I call IVL the great equalizer.
Dr. Dean Kereiakes is a paid consultant for Shockwave Medical.
Coronary Important Safety Information:
In the United States: Rx only.
Indications for Use—The Shockwave Intravascular Lithotripsy (IVL) System with the Shockwave C2 Coronary IVL Catheter is indicated for lithotripsy-enabled, low-pressure balloon dilatation of severely calcified, stenotic de novo coronary arteries prior to stenting.
Contraindications—The Shockwave C2 Coronary IVL System is contraindicated for the following: This device is not intended for stent delivery. This device is not intended for use in carotid or cerebrovascular arteries.
Warnings— Use the IVL Generator in accordance with recommended settings as stated in the Operator’s Manual. The risk of a dissection or perforation is increased in severely calcified lesions undergoing percutaneous treatment, including IVL. Appropriate provisional interventions should be readily available. Balloon loss of pressure was associated with a numerical increase in dissection which was not statistically significant and was not associated with MACE. Analysis indicates calcium length is a predictor of dissection and balloon loss of pressure. IVL generates mechanical pulses which may cause atrial or ventricular capture in bradycardic patients. In patients with implantable pacemakers and defibrillators, the asynchronous capture may interact with the sensing capabilities. Monitoring of the electrocardiographic rhythm and continuous arterial pressure during IVL treatment is required. In the event of clinically significant hemodynamic effects, temporarily cease delivery of IVL therapy.
Precautions— Only to be used by physicians trained in angiography and intravascular coronary procedures. Use only the recommended balloon inflation medium. Hydrophilic coating to be wet only with normal saline or water and care must be taken with sharp objects to avoid damage to the hydrophilic coating. Appropriate anticoagulant therapy should be administered by the physician. Precaution should be taken when treating patients with previous stenting within 5mm of target lesion.
Potential adverse effects consistent with standard based cardiac interventions include– Abrupt vessel closure – Allergic reaction to contrast medium, anticoagulant and/or antithrombotic therapy-Aneurysm-Arrhythmia-Arteriovenous fistula-Bleeding complications-Cardiac tamponade or pericardial effusion-Cardiopulmonary arrest-Cerebrovascular accident (CVA)-Coronary artery/vessel occlusion, perforation, rupture or dissection-Coronary artery spasm-Death-Emboli (air, tissue, thrombus or atherosclerotic emboli)-Emergency or non-emergency coronary artery bypass surgery-Emergency or non-emergency percutaneous coronary intervention-Entry site complications-Fracture of the guide wire or failure/malfunction of any component of the device that may or may not lead to device embolism, dissection, serious injury or surgical intervention-Hematoma at the vascular access site(s)-Hemorrhage-Hypertension/Hypotension-Infection/sepsis/fever-Myocardial Infarction-Myocardial Ischemia or unstable angina-Pain-Peripheral Ischemia-Pseudoaneurysm-Renal failure/insufficiency-Restenosis of the treated coronary artery leading to revascularization-Shock/pulmonary edema-Slow flow, no reflow, or abrupt closure of coronary artery-Stroke-Thrombus-Vessel closure, abrupt-Vessel injury requiring surgical repair-Vessel dissection, perforation, rupture, or spasm. Risks identified as related to the device and its use: Allergic/immunologic reaction to the catheter material(s) or coating-Device malfunction, failure, or balloon loss of pressure leading to device embolism, dissection, serious injury or surgical intervention-Atrial or ventricular extrasystole-Atrial or ventricular capture.
Prior to use, please reference the Instructions for Use for more information on warnings, precautions and adverse events. https://shockwavemedical.com/IFU
Please contact your local Shockwave representative for specific country availability and refer to the Shockwave C2 instructions for use containing important safety information.