RA vs OA: A Surprising Outcome in DIRO?
As one of the biggest calcium publications of 2023, JACC: Cardiovascular Interventions’ inclusion of the “Direct Comparison of Rotational vs Orbital Atherectomy for Calcified Lesions Guided by Optical Coherence Tomography” study, also known as DIRO, was notable as the first prospective randomized trial comparing rotational atherectomy (RA) and orbital atherectomy (OA). In the below Q&A, we invited its lead author Dr. Naotaka Okamoto of Osaka Rosai Hospital in Osaka, Japan to share his interpretation of the findings, how the results may impact the role of RA and OA in the cath lab, and the possibility of future research on the topic.
What makes the DIRO study unique?
Dr. Okamoto: The DIRO study is the first prospective randomized trial to compare the OCT findings and clinical outcomes in patients treated with rotational atherectomy (RA) versus orbital atherectomy (OA). All procedures were performed under OCT guidance in this study. While there are several previous studies comparing OCT findings and clinical outcomes after RA and OA, they were retrospective, and not all PCIs were performed with OCT. Therefore, the “prospective” and “OCT-guided” aspects of the DIRO study are unique points.
What were the key findings of the DIRO study and what key factors do you think led to them?
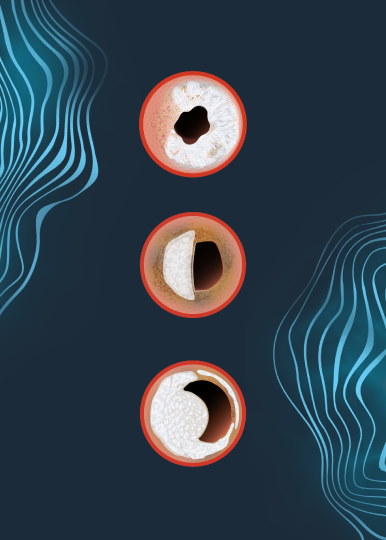
Dr. Okamoto: In this study, we analyzed both pre- and post-atherectomy OCT images to evaluate accurate and pure tissue modification resulting from atherectomy devices, and we observed greater tissue modification after RA compared to OA. Interventional cardiologists familiar with IVUS or OCT might have the impression that RA can achieve larger tissue modification than OA. However, not many interventional cardiologists are familiar with intracoronary imaging. For them, the result can be surprising. Furthermore, the finding that greater stent expansion resulted in larger tissue modification after RA than OA was surprising to me.
Do the study results align with what you personally experience in clinical practice?
Dr. Okamoto: As I mentioned above, I have the impression that RA can achieve larger tissue modification than OA and the DIRO study confirmed my impression. Furthermore, the finding that a bigger burr of RA can create a bigger tissue modification aligns with my experience.
Has DIRO generated any follow-on research ideas?
Dr. Okamoto: Yes, we are considering substudies of the DIRO study. For example, exploring the risk factors of slow-flow phenomenon and relevant factors of stent under-expansion after adequate tissue modification could be interesting. Additionally, comparison OCT findings after IVL, RA and OA is also intriguing, and we are currently prospectively collecting OCT images after IVL.
Given the findings of the study, are there certain clinical situations that you would still advocate for the use of OA over RA despite its decreased tissue modification ability?
Dr. Okamoto: Rotational atherectomy (RA) and orbital atherectomy (OA) are approaches to reduce calcium volume, and the DIRO study demonstrated that RA can eliminate more calcium. RA is favorable according to this result, but the DIRO study also demonstrated that RA tended to cause slow or no flow immediately after atherectomy compared with OA. This is probably explained by 3 reasons: 1) the amount of ablated plaque was small with OA; 2) OA is not likely to lead to burr wedge during atherectomy, because of its small burr size; and 3) OA can modify only target calcified lesions, whereas RA with large burr occasionally modifies not only target calcified lesions but proximal diseased lesions, even when they contain elastic tissue. Therefore, there is a stage at which OA plays an active role, especially for patients with a low ejection fractions or the last remaining coronary artery after old myocardial infarction, in whom slow or no flow can be critical even if it is transient.
Okamoto, N., Egami, Y., Nohara, H., Kawanami, S., Sugae, H., Kawamura, A., Ukita, K., Matsuhiro, Y., Nakamura, H., Yasumoto, K., Tsuda, M., Matsunaga-Lee, Y., Yano, M., Nishino, M., & Tanouchi, J. (2023). Direct comparison of rotational vs orbital atherectomy for calcified lesions guided by optical coherence tomography. JACC: Cardiovascular Interventions, 16(17), 2125–2136. https://doi.org/10.1016/j.jcin.2023.06.016
Views expressed are those of the author and not necessarily those of Shockwave Medical.
Dr. Naotaka Okamoto is a paid consultant for Shockwave Medical. See Important Safety information below.
Coronary Important Safety Information:
In the United States: Rx only
Indications for Use— The Shockwave Intravascular Lithotripsy (IVL) System with the Shockwave C2+ Coronary IVL Catheter is indicated for lithotripsy-enabled, low-pressure balloon dilatation of severely calcified, stenotic de novo coronary arteries prior to stenting.
Contraindications— The Shockwave C2+ Coronary IVL System is contraindicated for the following: This device is not intended for stent delivery. This device is not intended for use in carotid or cerebrovascular arteries.
Warnings—Use the IVL Generator in accordance with recommended settings as stated in the Operator’s Manual. The risk of a dissection or perforation is increased in severely calcified lesions undergoing percutaneous treatment, including IVL. Appropriate provisional interventions should be readily available. Balloon loss of pressure was associated with a numerical increase in dissection which was not statistically significant and was not associated with MACE. Analysis indicates calcium length is a predictor of dissection and balloon loss of pressure. IVL generates mechanical pulses which may cause atrial or ventricular capture in bradycardic patients. In patients with implantable pacemakers and defibrillators, the asynchronous capture may interact with the sensing capabilities. Monitoring of the electrocardiographic rhythm and continuous arterial pressure during IVL treatment is required. In the event of clinically significant hemodynamic effects, temporarily cease delivery of IVL therapy.
Precautions— Only to be used by physicians trained in angiography and intravascular coronary procedures. Use only the recommended balloon inflation medium. Hydrophilic coating to be wet only with normal saline or water and care must be taken with sharp objects to avoid damage to the hydrophilic coating. Appropriate anticoagulant therapy should be administered by the physician. Precaution should be taken when treating patients with previous stenting within 5mm of target lesion.
Potential adverse effects consistent with standard based cardiac interventions include– Abrupt vessel closure – Allergic reaction to contrast medium, anticoagulant and/or antithrombotic therapy-Aneurysm-Arrhythmia-Arteriovenous fistula-Bleeding complications-Cardiac tamponade or pericardial effusion-Cardiopulmonary arrest-Cerebrovascular accident (CVA)-Coronary artery/vessel occlusion, perforation, rupture or dissection-Coronary artery spasm-Death-Emboli (air, tissue, thrombus or atherosclerotic emboli)-Emergency or nonemergency coronary artery bypass surgery-Emergency or nonemergency percutaneous coronary intervention-Entry site complications-Fracture of the guide wire or failure/malfunction of any component of the device that may or may not lead to device embolism, dissection, serious injury or surgical intervention-Hematoma at the vascular access site(s)- Hemorrhage-Hypertension/Hypotension-Infection/sepsis/fever-Myocardial Infarction-Myocardial Ischemia or unstable angina-Pain-Peripheral Ischemia-Pseudoaneurysm-Renal failure/insufficiency-Restenosis of the treated coronary artery leading to revascularization-Shock/pulmonary edema-Slow flow, no reflow, or abrupt closure of coronary artery-Stroke Thrombus-Vessel closure, abrupt-Vessel injury requiring surgical repair-Vessel dissection, perforation, rupture, or spasm.
Risks identified as related to the device and its use: Allergic/immunologic reaction to the catheter material(s) or coating-Device malfunction, failure, or balloon loss of pressure leading to device embolism, dissection, serious injury or surgical intervention-Atrial or ventricular extra systole-Atrial or ventricular capture.
Prior to use, please reference the Instructions for Use for more information on indications, contraindications, warnings, precautions and adverse events. https://shockwavemedical.com/IFU