Shockwave Coronary IVL Reimbursement
Going deep into Shockwave Coronary IVL reimbursement: Since the launch of Coronary IVL in early 2021, Shockwave has made significant progress in establishing reimbursement for hospitals and physicians.
Shockwave Coronary IVL Physician Reimbursement
In calendar year 2024 (CY2024), The Centers for Medicare & Medicaid Services (CMS) established relative value units (RVUs) and associated payment for Current Procedural Terminology (CPT®)1 +92972, a Category I Add-on code for procedures involving Coronary IVL. For calendar year 2025 (CY2025), CPT® +92972 will continue to provide an additional 2.97 work RVUs and $139 payment in addition to the primary procedure effective January 1, 2025.
Shockwave Coronary IVL CPT® Code +92972 in CY2025
| CPT | Description | Additional Work RVUs2 | Additional Physician Facility Payment2,3 |
| +92972 | Percutaneous transluminal coronary lithotripsy | +2.97 | $139 |
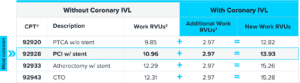
Application & Impact of Shockwave Coronary IVL CPT Code +92972
The tables below provide examples of how utilizing Coronary IVL and reporting CPT® code +92972 in conjunction with a primary procedure code impacts the total work RVUs and physician payment associated with a procedure.
CPT® code +92972 is an add-on code and may be used with all primary CPT® codes for PCI. For a complete description of appropriate use of +92972, please refer to the most current edition of the CPT® codebook from AMA CPT® Editorial Panel. The tables below describe the impact that +92972 has on the primary PCI procedure codes with which Coronary IVL is most frequently utilized. The RVUs and payment associated associated with +92972 are in addition to payments associated with the primary procedure.
Impact on Work RVUs When Shockwave Coronary IVL is Performed
Impact on Payment When Shockwave Coronary IVL is Performed

1: CPT only © 2024 American Medical Association. All rights Reserved.
2: CMS-1807-F; Medicare Physician Fee Schedule, MPFS, Calendar Year 2025 Final Rule. 11/01/24, Addendum B, using conversion factor 32.3465.
3: Payment rates do not take into account geographical or additional adjustments. Providers should contact their local Medicare Administrative Contractor (MAC) or CMS for specific information as payment rates vary by region.
Shockwave Coronary IVL Hospital Reimbursement
Hospital Inpatient Coding & Payments for Coronary IVL
Medicare reimburses inpatient care under the fiscal year 2025 (FY2025) Inpatient Prospective Payment System (IPPS) which utilizes the Medicare Severity Diagnosis Related Groups (MS-DRG) system for payment. Effective fiscal year 2024 (FY2024), when Coronary IVL is performed in the hospital inpatient setting with or without stent placement (any type), facilities are assigned one of the MS-DRG codes listed below. Performance of additional procedures may change the MS-DRG assignment. The below FY2025 payments for Coronary IVL MS-DRGs 323, 324 and 325 are effective starting October 1, 2024.
As compared to FY2024, the updated FY2025 payments associated with Coronary IVL procedures have increased by ~$1,650 on a volume weighted average basis.
Accordion Section
The following International Classification of Diseases Procedure Code (ICD-10-PCS) codes are specific to hospital inpatient procedures involving the use of Shockwave IVL on one or more coronary arteries. Codes associated with stent procedures as well any other procedures performed may also be applicable. Coronary IVL ICD-10-PCS codes must be billed in order to obtain Shockwave IVL MS-DRGs.
| ICD-10-PCS | Descriptor |
| 02F03ZZ | Fragmentation in coronary artery, one artery, percutaneous approach |
| 02F13ZZ | Fragmentation in coronary artery, two arteries, percutaneous approach |
| 02F23ZZ | Fragmentation in coronary artery, three arteries, percutaneous approach |
| 02F33ZZ | Fragmentation in coronary artery, four or more arteries, percutaneous approach |
Hospital Outpatient Coding & Payments for Shockwave Coronary IVL
CPT® code +92972 is an add-on code that must be used in conjunction with a designated primary procedure CPT® code as well as with the Coronary IVL Healthcare Common Procedure Coding System (HCPCS) code C1761. While both codes are packaged with the primary procedure, both must be billed in conjunction with the primary procedure(s) performed. A list of primary procedure codes commonly used with Coronary IVL can be found in the table below.
![Graphic showing hospital outpatient coding for Shockwave coronary IVL. Text reads Primary (J1) Procedure Code(s) [example: C9600 (PCI with Stent)] + C1761 (Coronary IVL HCPCS Code) + +92972 (Coronary IVL CPT Add-on Code](https://shockwavemedical.com/wp-content/uploads/2024/12/Hospital_Outpatient_Coding_Website_Coronary_IVL_Reimbursement_1000px-300x216.png)
Primary CPT® Procedure Codes Commonly Used with Shockwave Coronary IVL
| CPT®1 Code | Description | APC/Status Indicator2 | 2025 National Average Payment3 |
| 92920 | Percutaneous transluminal coronary angioplasty; single major coronary artery or branch | 5192/J1 | $5,702 |
| 92924 | Percutaneous transluminal coronary atherectomy, with coronary angioplasty when performed; single major coronary artery or branch | 5193/J1 | $11,341 |
| 92928 | Percutaneous transcatheter placement of intracoronary stent(s), with coronary angioplasty when performed; single major coronary artery or branch | 5193/J1 | $11,341 |
| 92933 | Percutaneous transluminal coronary atherectomy, with intracoronary stent, with coronary angioplasty when performed; single major coronary artery or branch | 5194/J1 | $17,957 |
| 92937 | Percutaneous transluminal revascularization of or through coronary artery bypass graft (internal mammary, free arterial, venous), any combination of intracoronary stent, atherectomy and angioplasty, including distal protection when performed; single vessel | 5193/J1 | $11,341 |
| 92941 | Percutaneous transluminal revascularization of acute total/subtotal occlusion during acute myocardial infarction, coronary artery or coronary artery bypass graft, any combination of intracoronary stent, atherectomy and angioplasty, including aspiration thrombectomy when performed, single vessel | Inpatient only | N/A |
| 92943 | Percutaneous transluminal revascularization of chronic total occlusion, coronary artery, coronary artery branch, or coronary artery bypass graft, any combination of intracoronary stent, atherectomy and angioplasty; single vessel | 5193/J1 | $11,341 |
| 92975 | Thrombolysis, coronary; by intracoronary infusion, including selective coronary angiography | Inpatient only | N/A |
| C9600 | Percutaneous transcatheter placement of drug eluting intracoronary stent(s), with coronary angioplasty when performed; single major coronary artery or branch | 5193/J1 | $11,341 |
| C9602 | Percutaneous transluminal coronary atherectomy, with drug eluting intracoronary stent, with coronary angioplasty when performed; single major coronary artery or branch | 5194/J1 | $17,957 |
| C9604 | Percutaneous transluminal revascularization of or through coronary artery bypass graft (internal mammary, free arterial, venous), any combination of drug-eluting intracoronary stent, atherectomy and angioplasty, including distal protection when performed; single vessel | 5193/J1 | $11,341 |
| C9606 | Percutaneous transluminal revascularization of acute total/subtotal occlusion during acute myocardial infarction, coronary artery or coronary artery bypass graft, any combination of drug-eluting intracoronary stent, atherectomy and angioplasty, including aspiration thrombectomy when performed, single vessel | Inpatient only | N/A |
| C9607 | Percutaneous transluminal revascularization of chronic total occlusion, coronary artery, coronary artery branch, or coronary artery bypass graft, any combination of drug-eluting intracoronary stent, atherectomy and angioplasty; single vessel | 5194/J1 | $17,957 |
1: CPT® only copyright 2024 American Medical Association. All rights Reserved.
2: Per Addendum D1, CY2025 OPPS Final Rule, Status Indicator J1 = Hospital Part B Services Paid Through a Comprehensive APC with the following payment status: all covered Part B services on the claim are packaged with the primary “J1” service for the claim, except services with OPPS status indicator of “F”,”G”, “H”, “L” and “U”; ambulance services; diagnostic and screening mammography; rehabilitation therapy services; services assigned to a new technology APC; self-administered drugs; all preventive services; and certain Part B inpatient services.
3: CMS-1809-FC; Medicare Hospital Outpatient Prospective Payment System (OPPS) Calendar Year 2025 Final Rule, Addendum B, 11122024. Payment rates do not take into account geographical or additional adjustments. Providers should contact their local Medicare Administrative Contractor (MAC) or CMS for specific information as payment rates vary by region.
Third party reimbursement amounts for specific procedures will vary by payer and by locality. This information is current as of November 2024 but is subject to change without notice. Amounts do not reflect any subsequent changes in payment since publication. To confirm reimbursement rates, you should consult with your local MAC for specific codes. Providers should select the most appropriate HCPCS code(s) with the highest level of detail to describe the service(s) rendered to the patient. Any questions should be directed to the pertinent local payer.
The coding, coverage, and payment information contained herein is gathered from various resources and is subject to change without notice. Shockwave Medical cannot guarantee success in obtaining third-party insurance payments. Third-party payment for medical products and services is affected by numerous factors. It is always the provider’s responsibility to determine and submit appropriate codes, charges, and modifiers for services that are rendered. Providers should contact their third-party payers for specific information on their coding, coverage, and payment policies.