BALI Makes Big Waves Demonstrating IVL Benefit in First Randomized Trial Showing Superiority Over Conventional Balloon-based Strategy
Unique Randomized Controlled Trial (RCT) Design Relevant for Clinical Practice
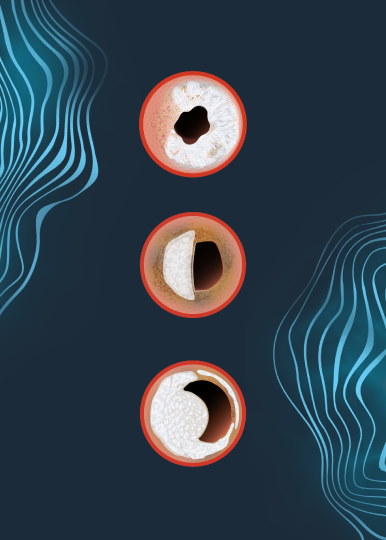
The BALI study is the first randomized study that examines the potential advantages of a routine Intravascular Lithotripsy (IVL) strategy versus conventional lesion preparation strategies in a rigorous, intracoronary imaging-guided, all-comers population with severely calcified lesions representative of real-world clinical practice.
- Recognizing that many calcium tools are complementary and atherectomy is a critical tool to be able to cross lesions, BALI compared 99 patients treated with IVL, 101 patients undergoing conventional balloon-based lesion preparation strategies, including cutting, scoring, ultra-high pressure balloons, and non-compliant (NC) balloons, but not IVL, across nine sites in Denmark, Norway, Estonia and Belgium.
- Rotational atherectomy was utilized in 31% of patients in the IVL arm and 42% of patients in the conventional lesion preparation arm only to facilitate balloon crossing.
Watch the BALI Trial Summary to learn why this study is important and for details on the study design and results.
Routine use of IVL Strategy Found Superior to Conventional Approaches
- 2/3 of patients with routine IVL were free of the primary endpoint, compared with approximately 1/2 of patients with conventional treatment arm, leading the BALI investigators to determine that at one year, a routine IVL strategy was the superior calcium modification strategy.
- The primary endpoint of procedural failure (stent implantation with a residual area stenosis of ≥20%) or target vessel failure (CD, TVMI CD-TLR) at one year occurred in 35% of IVL patients and in 52% of conventional preparation patients (psuperiority = 0.02).
| Lithotripsy (n=99) | Conventional (n=101) | p | |
| Primary Endpoint | 35.4% | 51.5% | 0.02 |
| Failed or no stent delivery | 1.0% | 0.0% | – |
| Residual area stenosis ≥20% (OCT) | 32.3% | 44.6% | – |
| Target vessel failure at 1 year | 4.0% | 10.9% | – |
| Cardiac death | 0.0% | 1.0% | – |
| Myocardial infarction | 3.0% | 5.9% | – |
| Clinically driven revascularization | 4.0% | 5.0% | – |
Watch Dr. Niels Thue Olsen, MD, PhD, Clinical Associate Professor at the University of Copenhagen, and Chief Medical Officer at Shockwave Medical, Nick West, discuss more about the BALI study.
Key Takeaway
In patients undergoing percutaneous coronary intervention (PCI) for severely calcified coronary lesions, the use of lithotripsy before stent implantation reduced the incidence of procedural failure or target vessel failure at one year, without an increased risk of adverse events.
Dr. Niels Thue Olsen is a paid consultant of Shockwave Medical.
Views expressed are those of the authors and not necessarily those of Shockwave Medical.