Shockwave Javelin: Severe TPT Stenosis, AT & PT Occlusion Case Review with Dr. Lendel
In this Shockwave Javelin case review, Dr. Vasili Lendel, Interventional Cardiologist at Arkansas Heart Hospital, Little Rock, AR, reviews a clinical case involving a patient with severe tibial peroneal (TP) trunk stenosis and anterior and posterior tibial occlusions, before diving into a Q&A discussion about Shockwave Javelin.
Case Summary
Patient background:
- 79-year-old male with a history of paroxysmal atrial fibrillation (PAF), hypertension, chronic kidney disease and type II diabetes
- Resting pain; symptoms remained refractory despite maximal medical and physical therapy
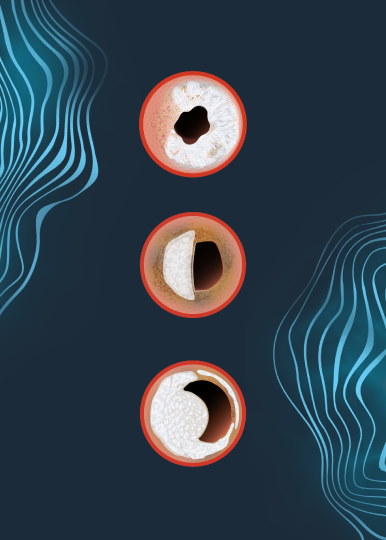
- Computed tomographic angiography (CTA) showed occluded anterior tibial (AT) artery, severe stenosis of the TP trunk with occluded posterior tibial artery (PT)
- Renovascular disease (RVD): 2.5 – 3 mm
- Lesion length: 120 mm
Treatment algorithm:
- 6 Fr 90 cm sheath
- 0.014″ guidewire was advanced into the distal PT
- Unable to advance 0.014 support catheter
- Shockwave Javelin was chosen to help cross and modify the calcified lesion
Treatment:
- Unable to cross the distal cap using Gaia next 3 and Astato XS 20 wires
- Shockwave Javelin was replaced for 0.018″ Crosswalk
- Retrograde access was obtained via distal PT artery using ultrasound
- Antegrade catheter was cannulated using retrograde Sion black wire
- Shockwave Javelin brought to distal cap and treated with the remaining pulses
- Subsequently, the artery was treated using 2.5 x 80 mm Shockwave E8, followed by 3 x 200 Armada balloon
Result:
- Brisk flow in the posterior tibial and medial plantar arteries without flow-limiting dissection
Dr. Lendel is a paid consultant of Shockwave Medical. The thoughts and views expressed are of their own opinions and do not necessarily represent Shockwave Medical.
Shockwave IVL: In the U.S.: Rx only. Prior to use, please reference the Important Safety Information for more information on indications, contraindications, warnings, precautions and adverse events.