New Data for Patients with Chronic Limb Threatening Ischemia (CLTI) with Dr. Venita Chandra
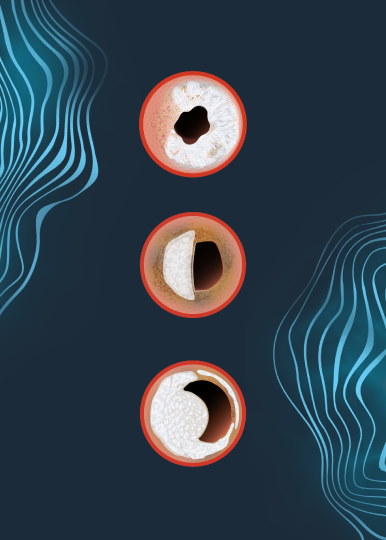
In this video, Dr. Venita Chandra shares 12-month outcomes from the DISRUPT BTK II trial, a prospective study evaluating IVL in a cohort of 250 patients, 200 of which have chronic limb-threatening ischemia (CLTI)—a population that is often excluded from clinical studies due to disease complexity.
The presentation highlights key clinical findings, including freedom from low intervention rates, low major amputation rates, and meaningful improvements in quality of life and wound healing. These outcomes demonstrate durable results at 12 months in severely calcified, below-the-knee disease.
Together, the data shown in this video support IVL as a frontline calcium-modification strategy* and an important part of the treatment algorithm for CLTI, reinforcing its role in improving patient outcomes and reducing amputation risk.
Watch now to learn more about how IVL is impacting outcomes in patients with CLTI.
Dr. Venita Chandra is a paid consultant of Shockwave Medical.
*Frontline Strategy: The approach of utilizing IVL as the primary treatment method, implemented without the use of atherectomy. This strategy is backed by the BTK II data based on the percentage of procedures involving pre-dilatation and post-dilatation, as well as the proportion of stenting performed. Our BTK II data indicates a notably low usage of both pre-dilatation and post-stenting in these cases.
Shockwave IVL: In the U.S.: Rx only. Prior to use, please reference the Important Safety Information for more information on indications, contraindications, warnings, precautions and adverse events.